Gut-brain therapy
Natural strategies for treatment-resistant depression
If you’ve been told you have “treatment-resistant” depression or if you feel like nothing’s fully working it might be time to look somewhere completely different: your gut.
Depression remains a leading global cause of psychiatric disability, affecting over 350 million people worldwide. While conventional treatments such as psychotherapy and pharmacotherapy offer relief for some, a significant portion of individuals experience treatment-resistant depression (TRD) or discontinue therapy due to adverse side effects. As the understanding of depression evolves, a new area of exploration has gained attention among researchers and clinicians alike, and it’s our gut-brain axis.
This bidirectional system, which links the gastrointestinal tract and the central nervous system, influences:
Mood regulation
Immune function
Neurotransmitter activity
Mounting evidence suggests that using psychobiotics (probiotic strains with neuroactive effects) and synbiotics (a combination of probiotics and their supportive prebiotics) could serve as complementary or even primary therapeutic strategies for clinical depression.
If you’ve tried multiple treatments and still feel stuck, it may be worth asking your doctor to consider your gut health in relation to your mood.
This is the turning point for many of the people I work with. When everything else has failed, the missing piece is often the gut.
Microbiota and Mood
Recent studies show that individuals with major depressive disorder (MDD) often exhibit gut dysbiosis, characterized by reduced microbial diversity and altered populations of key microbial species.
This matters because:
Key microbes produce neurotransmitters like serotonin and GABA.
Gut inflammation feeds systemic inflammation, which worsens mood.
A weakened gut lining allows toxins to disrupt neuroendocrine function.
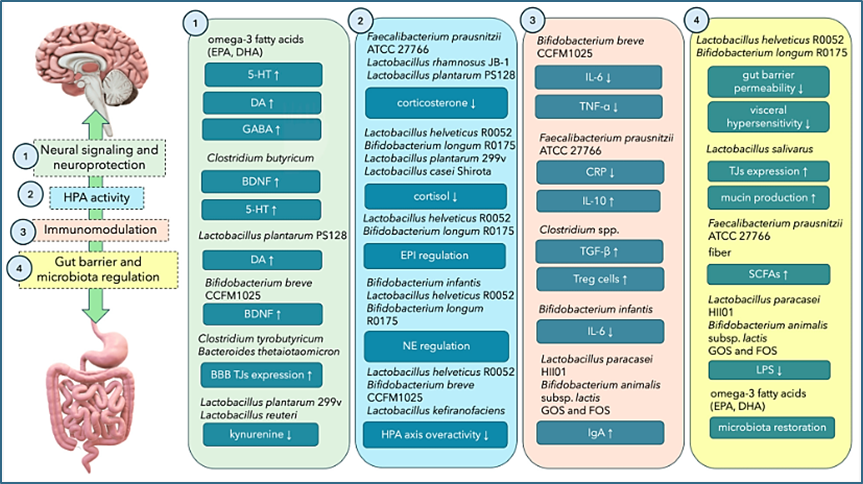
Probiotic strains, as illustrated in the image below, have shown promise in regulating the hypothalamic-pituitary-adrenal (HPA) axis, increasing the availability of key neurotransmitters, and reducing neuroinflammatory markers. Meanwhile, prebiotics such as fructooligosaccharides (FOS) and galactooligosaccharides (GOS) support these beneficial microbes by enhancing the production of short-chain fatty acids (SCFAs) and overall microbial balance.
Let’s get nerdy
Clinical findings suggest that synbiotics, particularly combinations such as Faecalibacterium prausnitzii ATCC 27766 with FOS and GOS, may offer superior benefits compared to individual probiotic or prebiotic interventions. In animal models and early human studies, these combinations have been shown to reduce depressive behaviors, improve gut integrity, and restore neurotransmitter levels.
Illustration: Overview of pathways of antidepressant effects on GABA axis via pro/prebiotics (Dziedzic et al., 2024)
Integrative Treatment Potential
Synbiotic and psychobiotic supplementation offers a low-risk, science-backed option that aligns with the principles of functional and personalized medicine. For treatment-resistant individuals who experience side effects from prescribed pharmaceuticals (SSRIs /SNRIs) or express interest in holistic care approaches, microbiome modulation can be a meaningful addition to the therapeutic plan.
It is essential to note that biotic therapies are not yet standardized. Strain specificity, dosage, and treatment duration vary widely across studies. Furthermore, microbiome profiles are highly individual. Providers considering the implementation of microbiome-targeted interventions should closely monitor outcomes and, where possible, tailor interventions based on gut health assessments or functional testing.
For clinicians, incorporating gut-brain axis strategies may complement dietary and lifestyle interventions, which are already part of many evidence-based mental health protocols. Emerging research also suggests that psychobiotics may enhance the efficacy of antidepressants and improve tolerability by stabilizing mood and reducing gastrointestinal side effects.
From Research to Practice
As our understanding of the biological roots of depression deepens, it is increasingly evident that mental health does not exist in isolation from other physiological systems. The gut-brain axis represents a promising frontier in depression care, where microbial interventions can influence mood, behavior, and neuroendocrine regulation. For mental health professionals and integrative health providers, psychobiotics and synbiotics offer practical, accessible tools to support the healing process, particularly in individuals unresponsive to conventional care. As research advances, incorporating microbiome-based strategies into mainstream mental health treatment protocols could transform outcomes and expand therapeutic possibilities.
In Conclusion
If you’ve tried everything: therapy, meds, mindset work, and you still don’t feel better, you may be missing a critical system check: your gut.
Even just tracking how you feel after meals, noting your energy, mood, and digestion for a week, can begin to map the gut-mind connection. It doesn't have to be perfect. Just start.
References
Averina, O. V., Poluektova, E. U., Zorkina, Y. A., Kovtun, A. S., & Danilenko, V. N. (2024). Human gut microbiota for diagnosis and treatment of depression. International Journal of Molecular Sciences, 25(11), 5782. https://doi.org/10.3390/ijms25115782
Chudzik, A., Orzyłowska, A., Rola, R., & Stanisz, G. J. (2024). Probiotics, prebiotics, and postbiotics on mitigation of depression symptoms: Modulation of the brain-gut–microbiome axis. Biomolecules, 11(7), 1000. https://doi.org/10.3390/biom11071000
Di Chiano, M., Sallustio, F., Fiocco, D., Rocchetti, M. T., Spano, G., Pontrelli, P., Moschetta, A., Gesualdo, L., Gadaleta, R. M., & Gallone, A. (2024). Psychobiotic properties of Lactiplantibacillus plantarum in neurodegenerative diseases. International Journal of Molecular Sciences, 25(17), 9489. https://doi.org/10.3390/ijms25179489
Dziedzic, A. Maciak, K., Bliźniewska-Kowalska, K., Gałecka, M., Kobierecka, W., & Saluk, J. (2024). The Power of Psychobiotics in Depression: A Modern Approach through the Microbiota-Gut-Brain Axis: A Literature Review. Nutrients, 16(7), 1054. Https://doi.org/10.3390/nu16071054
Hughes, R. L., Alvarado, D. A., Swanson, K. S., & Holscher, H. D. (2022). The prebiotic potential of inulin-type fructans: A systematic review. Advances in Nutrition, 13(2), 492–529. https://doi.org/10.1093/advances/nmab119
Kazemi, A., Noorbala, A. A., Azam, K., Eskandari, M. H., & Djafarian, K. (2019). Effect of probiotic and prebiotic vs placebo on psychological outcomes in patients with major depressive disorder: A randomized clinical trial. Clinical Nutrition, 38(2), 522–528. https://doi.org/10.1016/j.clnu.2018.04.010
Paiva, I. H. R., Maciel, L. M., Silva, R. S. D., Mendonça, I. P., Souza, J. R. B., & Peixoto, C. A. (2024). Prebiotics modulate the microbiota-gut-brain axis and ameliorate anxiety and depression-like behavior in HFD-fed mice. Food Research International, 182, 114153. https://doi.org/10.1016/j.foodres.2024.11415 3
Palepu, M. S. K., Bhalerao, H. A., Sonti, R., & Dandekar, M. P. (2024). Faecalibacterium prausnitzii, FOS, and GOS loaded synbiotic reverses treatment-resistant depression in rats: Restoration of gut-brain crosstalk. European Journal of Pharmacology, 983, 176960. https://doi.org/10.1016/j.ejphar.2024.176960
Yin, Y., Ju, T., Zeng, D., Duan, F., Zhu, Y., Liu, J., Li, Y., & Lu, W. (2024). "Inflamed" depression: A review of the interactions between depression and inflammation and current anti-inflammatory strategies for depression. Pharmacological Research, 207, 107322. https://doi.org/10.1016/j.phrs.2024.107322
Zhang, Q., Chen, B., Zhang, J., Dong, J., Ma, J., Zhang, Y., Jin, K., & Lu, J. (2023). Effect of prebiotics, probiotics, synbiotics on depression: Results from a meta-analysis. BMC Psychiatry, 23(1), 477. https://doi.org/10.1186/s12888-023-04963-x